Synovial osteochondromatosis is an idiopathic benign metaplasia of synovial membrane that typically occurs in the third to fifth decades of life. Manifestations are chronic joint pain and decreased range of motion of the involved joint. This disorder affects men about twice as often as women. It is almost always monoarticular, most commonly affecting the knee, hip, or elbow and less commonly, the wrist, ankle, and shoulder.' The various imaging manifestations of synovial osteochondromatosis detected on plain film radiography, arthrography, computed tomography (CT), and magnetic resonance imaging (MRI) have been well described.2*5 A review of the literature revealed only one previous report demonstrating the ultrasound (US) findings of synovial osteochondromatosis of the shoulder.6 Three additional case reports7-9 and one textbook example' have shown the US findings of this entity involving other synovial joints. Herein we report a case showing a high-quality example of the US appearance of synovial osteochondromatosis of the shoulder and include plain film radiographic, CT, and pathologic correlation.
A 46-year-old man sought medical advice from his local physician because of a nontender mass overlying his left shoulder associated with stiffness and decreased range of motion of the left glenohumeral joint. Physical examination confirmed a painless mass, 10 by 10 cm, overlying the left shoulder region. A soft tissue tumor, probably a lipoma, was clinically suspected.
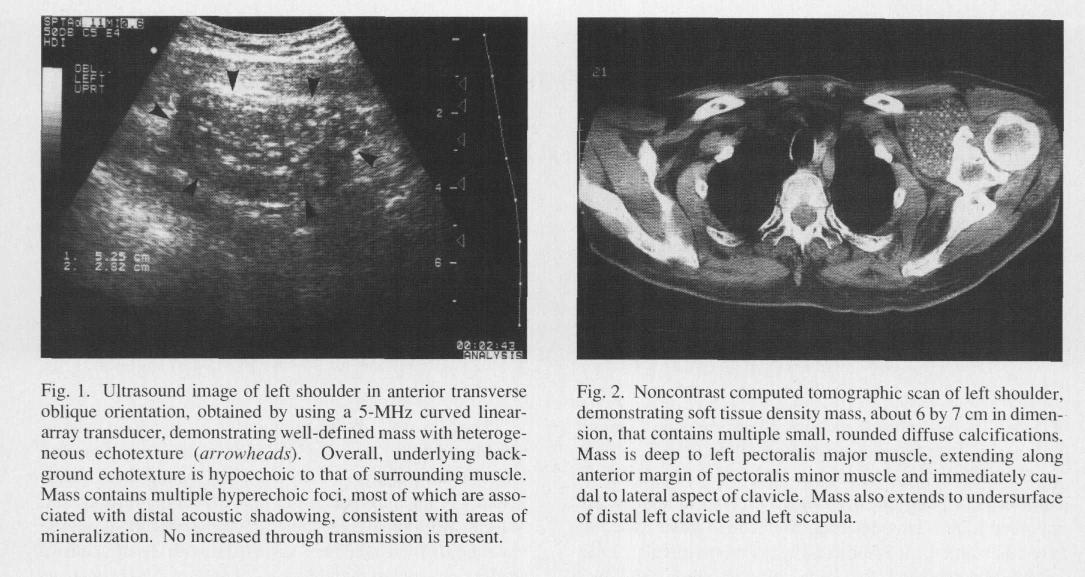
The mass was first imaged with US, which revealed a solid mass with heterogeneous echotexture anterior to the left shoulder (Fig. 1). Overall, the background echogenicity of the mass was lower than that of the surrounding muscle. Multiple hyperechoic foci were present within the mass, some of which were associated with distal acoustic shadowing, consistent with mineralization. The borders of the mass were well defined, and no increased through transmission was noted. Because of the presence of the multiple highly echogenic foci within the mass, the US findings did not support the referring clinician's suggestion of a lipoma, and MRI was recommended for further evaluation. The MRI examination was attempted but had to be terminated before any diagnostic images were obtained because of the patient's severe claustrophobia.
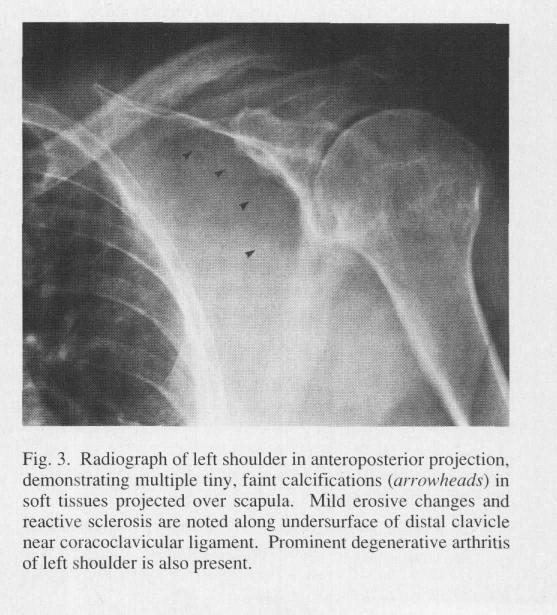
CT of the left shoulder without use of contrast material was then performed. This demonstrated a mass posterior to the left pectoralis major muscle, extending anterior to the pectoralis minor and immediately caudal to the lateral aspect of the clavicle (Fig. 2). The mass, about 6 by 7 cm in dimension, contained diffuse speckled calcifications and extended to the undersurface of the distal left clavicle and left scapula.
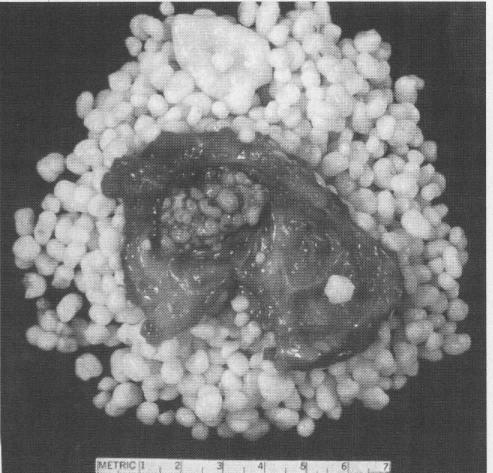
Radiographs of the left shoulder in anteroposterior internal (Fig. 3) and external rotation and axillary projections demonstrated multiple tiny, faint calcifications in the soft tissues anterior to the scapula. Some erosive changes and reactive sclerosis were noted in the clavicle in the region of the coracoclavicular ligament. Moderate to marked degenerative changes were also present in the glenohumeral joint.
Open excisional biopsy and synovectomy confirmed the diagnosis of synovial osteochondromatosis (Fig. 4). The patient experienced almost complete recovery after a 3week postoperative course of shoulder immobilization, followed by physical therapy that included range-of-motion exercises for the left shoulder. Two-year postoperative follow-up by both physical examination and plain film radiography demonstrated no evidence of recurrent synovial osteochondromatosis.
Because of recent renewed interest in the use of US in the evaluation of musculoskeletal disease, such as rotator cuff arthropathy11,12 or suspected intra-articular loose body,6 opportunities to diagnose synovial osteochondromatosis with this modality have become more frequent. The US features of synovial osteochondromatosis demonstrated in our case and in the previously reported cases6-10 include a well-circumscribed periarticular or intra-articular hypoechoic mass containing multiple echogenic foci, synovial membrane thickening, widening of the joint space, and secondary erosive and arthritic changes. These features are both consistent with and predicted by the expected pathologic changes of synovial osteochondromatosis. The US manifestations of synovial osteochondromatosis were first reported in 1984 by Moss and Dishuk,7 who used a static scanner in a case involving the popliteal fossa. Although pathologic verification was not provided in that case, double-contrast arthrographic findings were reported to be classic for this disease process. A US appearance of synovial osteochondromatosis involving the shoulder was shown in a recent article by Frankel and colleagues,' who studied the efficacy of US for the detection of intra-articular bodies. They examined 280 patients with symptoms in various synovial joints and concluded that US is an accurate method for identification of intra-articular bodies; these data support the increased use of US for the evaluation of suspected joint pathologic involvement.
Plain film radiography should remain the first study of choice in evaluating suspected soft tissue or skeletal masses. Radiographs, however, are not sensitive for detecting early changes of synovial osteochondromatosis; usually they show only joint space widening.' Our case report illustrates that the definitive diagnosis of synovial osteochondromatosis can be made with US and supports the use of this modality as an alternative to CT or MRI. Indeed, MRI could not be performed because of our patient's claustrophobia. About 5 to 10% of the general population cannot undergo MRI because of various reasons, including claustrophobia or presence of a cardiac pacemaker, other metallic medical implants, and imbedded metallic foreign bodies. For such patients, US seems to be a reasonable alternative to MRI. Recent datab2 support the increased use of US for the evaluation of clinically suspected joint pathology. The advantages of this technique are its relatively low cost, wide availability, noninvasiveness, absence of ionizing radiation, and real-time capability including the ability to manipulate the joint during the examination. The major drawback of US is its high operator dependence.
.com>
 典型病例分享
典型病例分享